One of the most common questions I get is “how do I study pharmacology?”
So, here are a few tips to help you more effectively and efficiently study pharmacology in nursing school….
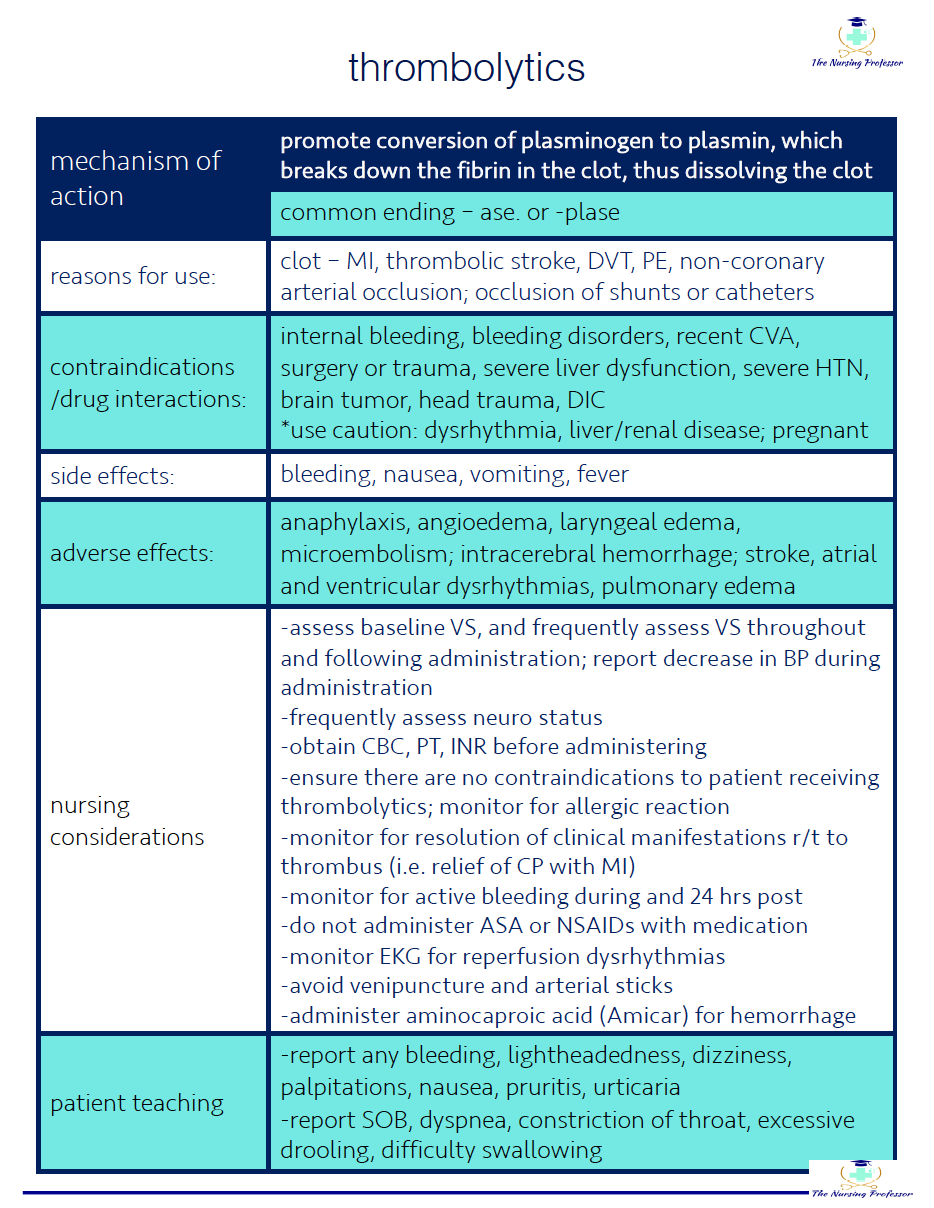
#1 - Initially, focus on learning commonalities within drug classes…then focus on the most common medications
You will definitely have to learn some individual medications, but understanding the ins and outs of the medication class, as opposed to trying to know every individual medication will save you a lot of time and energy. So first, master the medication classes, then spend time learning the most important info about the most common medications that you are likely to administer and see on NCLEX. (A list of these medications can be found in RN School and our Nursing Pharmacology course that we are currently building out.)
#2 - Know the common medication prefixes and suffixes for each drug class
Committing to memory the common endings that occur in drug classes can help you get a better overall feel for medications. For example, if your patient mentions that they take metoprolol - you can deduce that since it ends in -lol that this medication is probably a beta-blocker. If you followed tip #1, then you would know all about beta-blockers and would have an idea of what the med does, potential reasons the patient would be taking it, side effects and so on. (A common prefixes and suffixes cheatsheet can be found in RN School and our Nursing Pharmacology course that we are currently building out.)
#3 - focus on generic names
It is really tempting to learn brand names because they are typically what we are more familiar with and often easier to remember, but you will be faced with generic names on NCLEX…so it is definitely best to remember them.
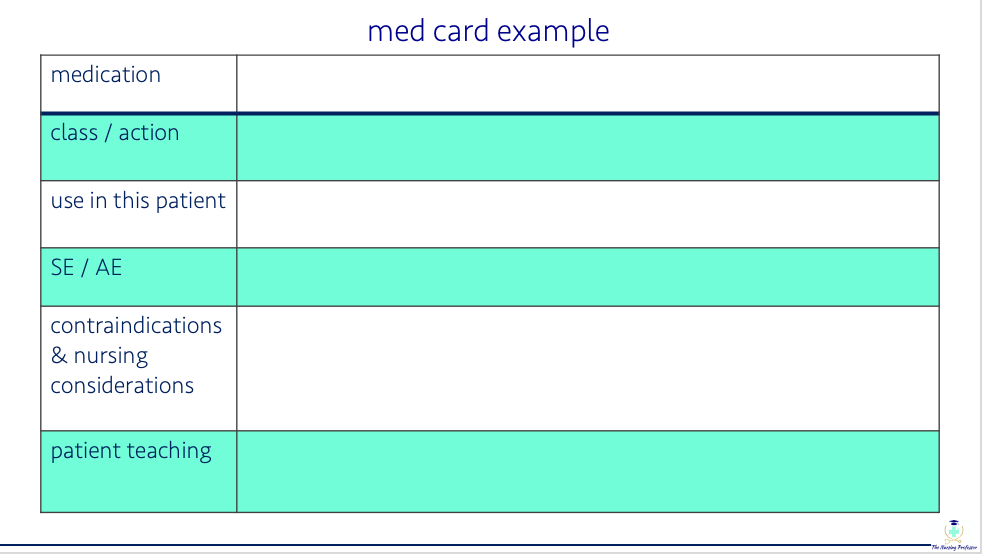
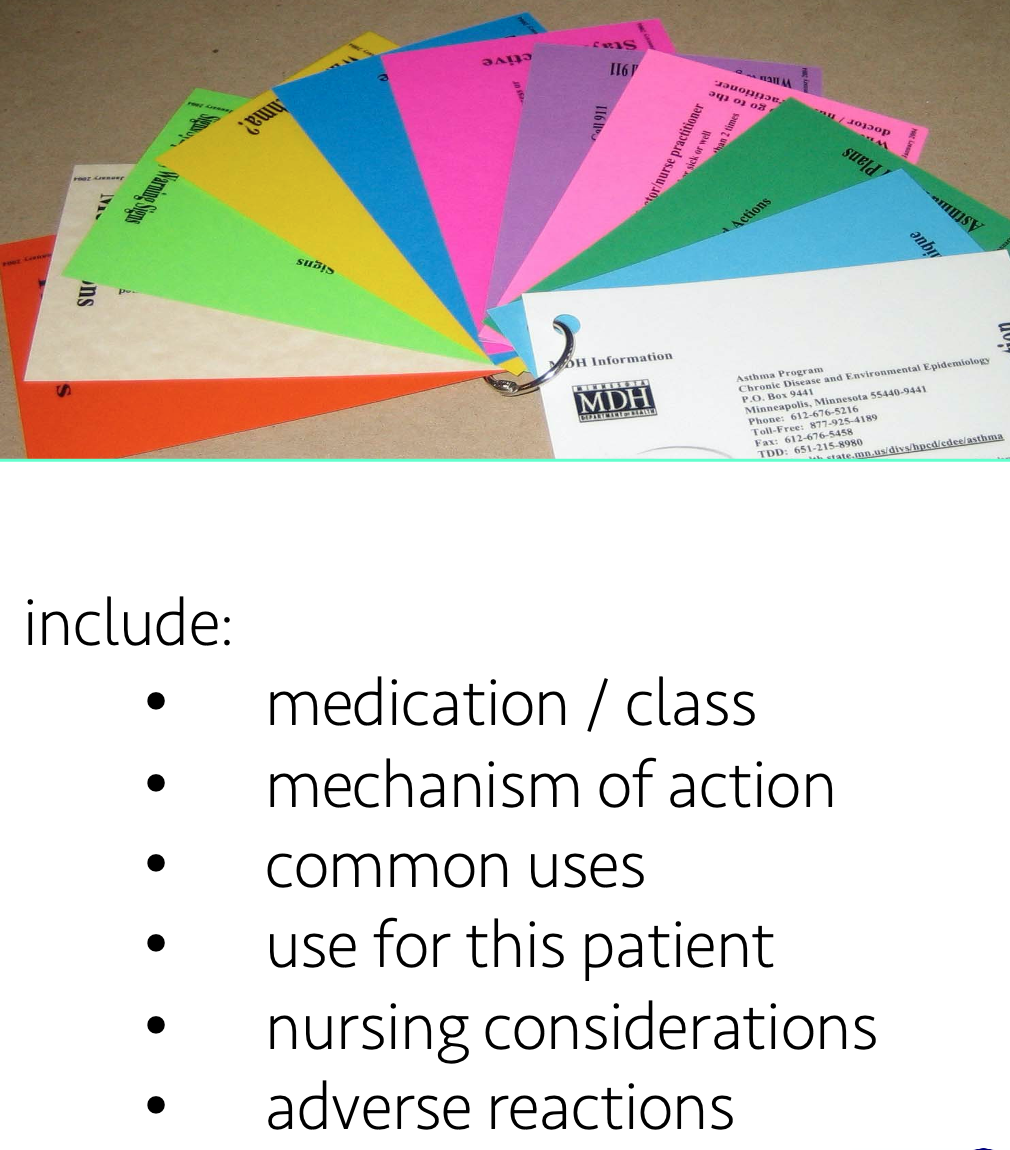
#4 - use medication cards or flash cards…but make your own
Making your own medication cards is one of the best things you can do to help you memorize your meds. First off, writing something down in your own hand helps your brain process it and commit it to memory (especially if you’ve written it down 3 times). But the great thing about medication cards is that you can take them with you to clinical and use them as you refresh on the medications that you are about to administer to your patient.
As a clinical instructor, I had my students make cards for the meds their patients were on each week. Each medication and it's’ information would be written on an index card and they would be kept together by a ring clip. They never had to re-create the card (because you know that so many patients in the hospital are on the exact same medications), they would only tweak it as needed depending on why their patient was taking it (i.e. reason for use in that patient might be different than the reason the previous patient was taking it). This way they could easily refresh on the med before it was time to give it to the patient and they could use them to quiz themselves or each other.
But again let me reiterate - if you are going to use med cards you should make them yourself. Trust me it will help. And if you are a highly visual person, then using a color method with your cards (and school notes) might help - for instance using red cards for cardiac meds, yellow for renal, etc.
#5 - one of my top tips for studying anything in nursing school, including pharmacology….
study systematically
I say this all of the time because (especially in nursing school) it is important and really helps - study systematically - meaning, always approach studying each medication in the same way.
For example,
start with the name and drug class
does it have a common ending?
what is the mechanism of action?
potential uses
side effects/adverse effects
contraindications
nursing considerations
patient teaching
If you study each med in the same systematic way you are less likely to forget something important and your brain thrives with repetition and routine.
i hope these tips help you master your medications!
and remember…
the ultimate way to remember medications is to actually administer them to your patients while in clinical. Look up your meds before you administer them every time until you have got them down!
Be sure to come back next Friday for another round of Pharmacology Friday!
For pharmacology templates, cheatsheets, practice questions and so much more, be sure to check out our membership, RN School, that has everything you need to Thrive in Nursing School! And keep an eye out for our Nursing Pharmacology Course which is coming soon!